
How Healthcare Leaders Can Thrive Amidst Constant Crisis
You feel it every day. The crushing pressure. The weight of impossible demands. The sheer personal cost of leading in a system that’s in a constant state of emergency. It's the soul-deep exhaustion from battling workforce shortages and navigating systemic failures, all while trying to show up for your team. The internal script is always running: "If I stop performing, if I drop a single ball, this whole thing falls apart."
Key Takeaways
The Leader's Physiological Tax: Constant crisis management, workforce shortages, and financial pressures are not just business problems; they are physiological withdrawals from your nervous system, leading to burnout and decision fatigue.
From Reactive to Sovereign: Traditional, top-down leadership is broken. The solution lies in a new paradigm that prioritizes nervous system regulation as a core strategic competency, allowing you to lead from a place of stability.
Inequity as an Operational Failure: Gaps in patient care are not just social issues. They create operational chaos, fuel staff burnout, and erode community trust, making them a critical leadership challenge to solve.
The RAMS Framework: A sustainable path forward requires a focus on four pillars: Redefined Results (beyond financials), proactive Attitude (nervous system regulation), personal Mastery (embodied skills), and resilient Systems (organizational design).
Acknowledging the Leader's Burden
The leadership challenges in healthcare are not just a series of operational problems; they are systemic pressures that levy a direct tax on your nervous system and personal well-being. Acknowledging this physiological cost is the first step toward shifting from a state of survival to one of sovereign, effective leadership.
The burden you carry is more than a heavy workload. It’s an accumulation of emotional, cognitive, and physical drains that build up in silence.
High-achieving women, in particular, often find themselves at this breaking point, where a career full of accolades masterfully hides a profound sense of isolation. It’s a common, yet rarely spoken of, part of the leadership journey that leads to a silent crisis for successful women, turning them into the loneliest leaders in the room.
This internal reality is shaped by a few distinct pressures you know all too well:
The Emotional Weight of Care Gaps: You carry a personal sense of responsibility for every gap in patient care, every delayed treatment, and every person who can't get the services they desperately need.
Constant Crisis Management: Your job has morphed from strategic leadership into perpetual firefighting. You're reacting, to staffing emergencies, budget cuts, and regulatory nightmares.
The Isolation of Authority: Everyone expects you to have all the answers and project unwavering strength. This pressure makes it almost impossible to show vulnerability or ask for the very support you need to keep going.
This pile-up of unvoiced pressures exacts a significant physiological tax. It isn't a sign of weakness; it's the predictable outcome of carrying an unsustainable load within a broken system. Simply acknowledging this reality is the first, most crucial step toward reclaiming your energy and learning to lead from a place of sovereignty, not just survival.
Defining Today's Leadership Challenges in Healthcare
The leadership challenges hitting healthcare right now aren't just operational speed bumps; they're systemic pressures that levy a direct tax on your nervous system. Every crisis, from a sudden staffing gap to another round of budget cuts, makes a withdrawal from your cognitive and emotional reserves. It’s a reality that makes traditional, top-down leadership models not just ineffective, but completely unsustainable.
These problems are tangled together, feeding into a vicious cycle of strain that ripples through every level of your organization. Seeing this dynamic for what it is, a web, not a list of separate issues, is the first real step toward breaking free from a constant state of reaction and starting to lead with clear intention.
The Core Crises Facing Healthcare Leaders
That feeling of being stretched to the breaking point? It’s not just in your head. It’s the direct result of three core crises colliding at once. These aren't isolated challenges you can tackle one by one; they amplify each other, creating a constant state of pressure that feels inescapable.
The primary drivers fueling this environment are:
Pervasive Workforce Shortages: The industry is bleeding qualified professionals, from nurses to highly trained specialists. This isn't a temporary dip; it's a structural crisis that overloads your remaining staff and directly compromises patient care.
Escalating Staff Burnout: Your teams are running on fumes. The relentless pace, the emotional weight of the work, and the high-stakes environment are causing burnout, disengagement, and sky-high turnover, which, of course, just makes the staffing crisis worse.
Intense Financial and Operational Pressure: You're being asked to do the impossible: improve patient outcomes and expand services while slashing costs and navigating shrinking budgets. This constant financial squeeze forces agonizing decisions that inevitably hit morale and resources hard.
This isn't just a series of unfortunate events. It's a system of interconnected burdens, shortages, demands, and burnout, that directly drains a leader's capacity to lead effectively.
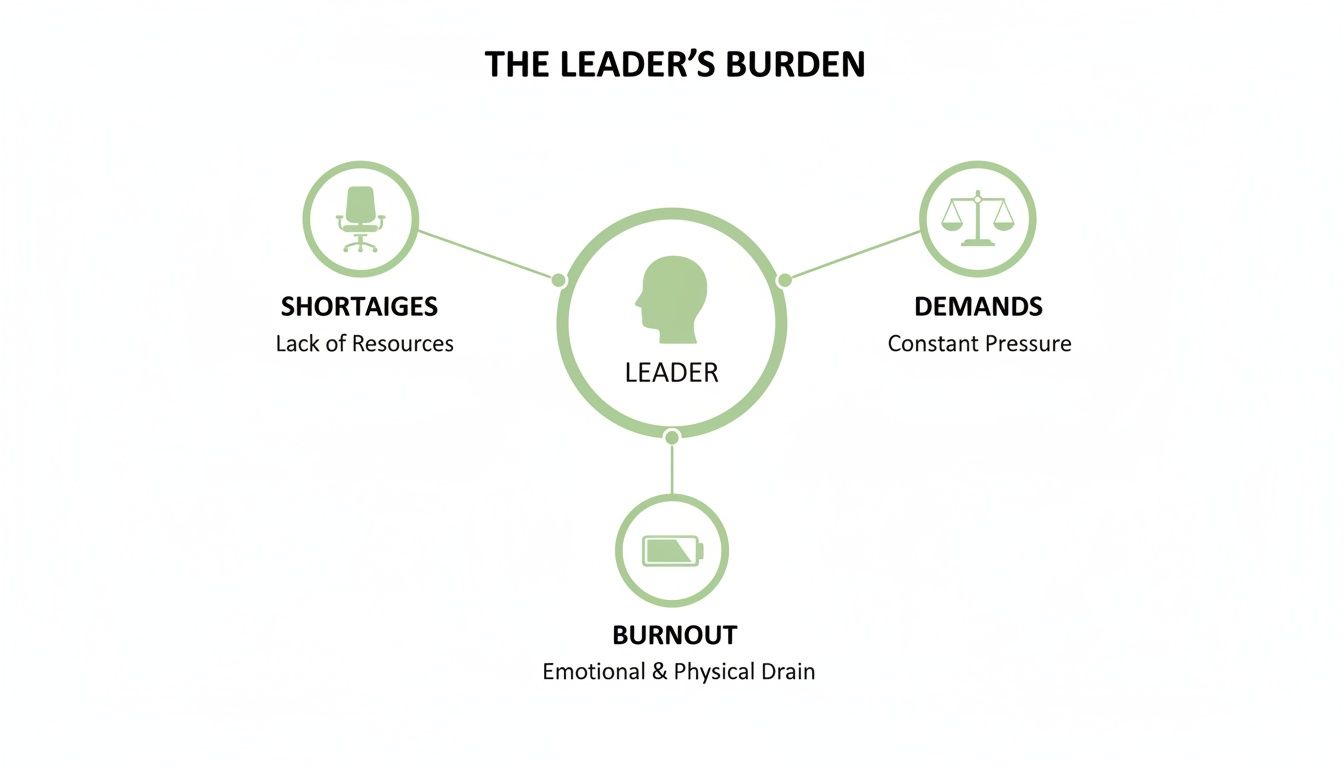
As the visual shows, you aren't just dealing with one problem. You're caught in a reinforcing loop of pressures that depletes both your personal energy and your organization's resources.
The Physiological Tax of Modern Healthcare Leadership
Think of each of these challenges as a physiological tax. Every unexpected resignation, every tense budget meeting, every patient complaint, each one makes a direct withdrawal from your nervous system’s bank account. Over time, these withdrawals empty your capacity for strategic thinking, emotional regulation, and decisive action.
You end up running on empty, trying to solve systemic problems with sheer force of will. But that's not a sustainable strategy. It’s precisely why so many brilliant, dedicated leaders feel stuck, exhausted, and powerless to create real change. They are paying an immense biological price for systemic dysfunction.
Tackling the severe workforce shortages and the resulting burnout has become the most urgent leadership challenge. Labor costs in US hospitals exploded by over $42.5 billion between 2021 and 2024, now sitting at a staggering $839 billion. This surge is fueled by an alarming exodus of talent, with an estimated 1 million nurses expected to retire by 2030 and a 50% jump in physician resignations between 2020 and 2024. Globally, the World Health Organization projects a shortfall of 10 million health workers by 2030.
The old model of leadership, push harder, absorb more pressure, and fix it all yourself, is officially broken. It treats the leader as an infinite resource, completely ignoring the very real biological cost of navigating a sustained crisis.
To truly fix these issues, we have to shift our focus. Instead of just managing the symptoms (like turnover and budget deficits), we need to address the root cause: a leadership approach that is dangerously misaligned with the physiological realities of the modern healthcare environment. This requires a new way of thinking, the kind detailed in effective healthcare leadership development programs that treat nervous system regulation as a core competency, not a soft skill.
This new leadership paradigm isn't about finding a magic bullet to solve staffing or budget crises overnight. It’s about building the internal capacity to lead with clarity, resilience, and sovereignty, even when the external world is chaotic. This journey starts by recognizing a fundamental truth: your well-being isn't a luxury. It is the central pillar of sustainable and effective leadership.
Old vs. New Healthcare Leadership Paradigms
The shift required is monumental. It's moving from a reactive, brute-force model to one that is proactive, strategic, and deeply aware of the human nervous system's role in performance and decision-making.

The traditional column reflects a leadership style that, while once common, now actively contributes to the very problems it seeks to solve. The Sovereign (RAMS) approach, in contrast, builds the capacity within the leader and the team to navigate complexity from a place of stability and strength.
How Inequity and Access Gaps Fuel the Crisis
Beyond the immediate fires of staffing shortages and budget cuts, there's a quieter, more corrosive leadership challenge eating away at healthcare: the destabilizing crisis of inequity. Gaps in care aren't just abstract social issues; they are operational failures that send chaotic ripples through your entire organization.
This is where the leader’s burden becomes intensely personal and frankly, exhausting. When systemic barriers prevent your teams from effectively serving entire communities, it does more than just strain resources. It demolishes trust, triggers profound moral injury, and traps you and your staff in a constant state of reactive damage control.

The Ripple Effect of Inaccessible Care
Think of your organization as a delicate ecosystem. When one part is starved, like communities facing care deserts or impossible wait times, the whole system teeters on the brink of collapse. These gaps don’t stay neatly contained. They show up as urgent operational problems that land squarely on your desk.
This isn't just a theory; it's a measurable crisis playing out in real-time. A recent worldwide survey found that a staggering 46% of adults believe access to treatment and long waits are the single biggest problem in healthcare. Another 45% point directly to staff shortages. With two billion people globally facing financial hardship from healthcare costs, the pressure is astronomical. You can learn more about these global healthcare findings on Statista.com.
The consequences are severe, predictable, and deeply interconnected:
Overwhelmed Emergency Services: When primary care is a fantasy, patients delay treatment. Minor issues become critical emergencies, flooding your ED and overwhelming a system that was never designed for that load.
Skyrocketing Burnout and Moral Injury: Your clinicians are left feeling powerless and ethically compromised. They know the right care exists, but they can't provide it to the people who desperately need it. That conflict is a primary driver of burnout.
Erosion of Community Trust: Inconsistent access sends a clear, painful message: the system isn't for you. This breakdown of trust makes every public health initiative, every outreach program, an uphill battle.
Every rural patient who can't see a specialist, every family agonizing over out-of-pocket costs—these are not just statistics. Each one represents a system failure that adds to the physiological and moral tax on your team. It’s an unwinnable fight that burns out your very best people.
From Social Issue to Leadership Mandate
Tackling inequity is no longer just the job of public health officials. For a healthcare leader, it has become a core strategic mandate. Why? Because failing to address these access gaps directly feeds the burnout and staffing crises you're already fighting tooth and nail.
You simply cannot claim to value your staff while forcing them into situations where they have to ration care or turn people away. The psychological dissonance is too great. This is where the principles of what is inclusive leadership become mission-critical. It's about consciously designing systems that distribute resources fairly, not just within your four walls, but across the entire community you serve.
Leading through this requires a profound shift in perspective. It means seeing community health not as an external variable but as a direct indicator of your own organization’s stability. It’s about moving beyond temporary fixes and fighting for systemic changes that make equitable care a reality. This isn’t just about "doing the right thing." It's about creating a sustainable operational environment where your teams can finally do their best work without carrying the moral weight of a fractured system on their shoulders.
The RAMS Framework: A New Path for Leaders
Let’s be honest. The constant cycle of putting out fires, battling staff shortages, slashing budgets, and plugging gaps in patient care, isn't a leadership strategy. It's a survival tactic. It's a reactive posture that torches your energy and your team's morale, leaving everyone feeling utterly powerless.
To break free, you need a completely new way of operating. You need a model built not on enduring chaos, but on creating stability from the inside out. This is precisely why the RAMS framework was created.
RAMS is a structured, intentional approach designed to pull you out of that constant state of reaction and into a state of regulated, purposeful leadership. It carves a clear path for tackling the tangled web of leadership challenges in healthcare by focusing on four interconnected pillars that build resilience, both in you and your entire organization.
R Is For Redefined Results
In the high-stakes world of healthcare, we've been conditioned to define "results" through a ridiculously narrow lens: financial performance, patient throughput, budget adherence. While these numbers matter, they don't tell the whole story. Not even close.
This blinkered view forces leaders into impossible corners, often pushing them to make choices that juice short-term metrics at the direct expense of long-term stability and the well-being of their people.
The very first step in the RAMS framework is to blow up this outdated definition of a "good result."
Sustainable Clinical Outcomes: This isn't just about discharge rates. It's about focusing on the long-term health of your patients and the well-being of the community you serve.
High Team Retention: Start seeing a stable, engaged workforce for what it is: a primary indicator of organizational health and your single most critical business asset.
Psychological Safety: How safe do your people feel to speak up, to innovate, to flag an error without fearing blame? This is a core metric of a healthy system.
Leader Well-being: Your own capacity and nervous system regulation aren't luxuries; they are direct inputs to your organization's success or failure.
When you broaden the definition of success, you fundamentally change the game. You start making different decisions. You invest in your people, not just your processes, and in doing so, you build a foundation for performance that actually lasts.
A Is For Attitude
Your attitude as a leader is so much more than your mood. It's the emotional and physiological frequency you broadcast to your entire team. When crisis hits, your team isn't just listening to your words—they're reading your nervous system.
A dysregulated, reactive leader creates a dysregulated, reactive team. Period. But a grounded, intentional leader creates a culture of stability, even when everything outside is spinning out of control.
The Attitude pillar is about making a conscious shift from a reactive state, driven by external chaos, to a proactive state guided by your own internal sovereignty. It’s the daily practice of managing your own physiology first so you can effectively co-regulate the collective nervous system of your organization.
This is about developing the capacity to absorb pressure without becoming the pressure. It’s about showing up with a calm, clear presence that signals safety and competence, giving your team the psychological fuel they need to perform at their absolute best.
M Is For Mastery
Mastery isn't about the technical skills you picked up in business school. It's about the deep, personal, embodied skills required to lead effectively when the pressure is immense. These are the competencies that shield you from burnout and allow you to make resilient decisions.
These are the skills that empower you to hold the line when everything and everyone is demanding more than you can possibly give.
Essential skills for Mastery in healthcare leadership include:
Boundary Setting: The ability to strategically say "no" to protect your energy and your team's focus, even when powerful stakeholders are demanding a "yes."
Resilient Decision-Making: The capacity to make clear, values-aligned choices under fire, without getting hijacked by stress or fear.
Emotional Regulation: The skill of processing high-stakes emotional data, from a critical incident report to a tense team conflict, without becoming overwhelmed yourself.
Mastery is your internal anchor. It's the personal work you do to guarantee you have the internal resources to meet the crushing external demands of your role, without sacrificing yourself in the process.
S Is For Systems
Finally, the Systems pillar brings it all together. It's about architecting the organizational structures, processes, and cultural norms that actively support your team. Too often, leaders try to solve systemic problems, like burnout or disengagement, with individual "fixes."
But here's the hard truth: no amount of wellness apps or yoga classes can fix a broken scheduling system or a toxic communication culture.
The RAMS approach is built on a simple premise: good people break down in bad systems. A leader's primary role, then, is to become an architect of better systems.
This means taking a hard, honest look at "the way we do things around here" and redesigning workflows that reduce friction instead of creating it. This could look like:
Streamlining communication channels to cut down on cognitive overload.
Implementing scheduling protocols that truly protect staff from chronic exhaustion.
Creating transparent, fair processes for allocating resources and making key decisions.
By focusing on Systems, you stop blaming individuals for systemic failures and start building an environment where your team is genuinely set up to win.
Applying the RAMS Method Where It Actually Counts
Theory is one thing; the chaotic reality of a twelve-hour shift is another. The real test of any leadership model isn’t how elegant it looks on paper, but how it holds up in the trenches. How does the RAMS Method actually translate into tangible, measurable change when you’re facing the relentless leadership challenges in healthcare?
This is where we move from the abstract to the actionable. The framework is a blueprint for shifting from a state of constant reaction to one of controlled, effective action. It gives you a clear path to dismantle the patterns driving burnout and operational failure, replacing them with structures that build genuine resilience.

Case Study One: Systems in Action to Combat Nurse Burnout
Let’s look at a hospital administrator, Sarah, who was grappling with a nurse turnover rate that had climbed to an alarming 30%. Her old approach was purely reactive, throwing sign-on bonuses at the problem and conducting exit interviews that all said the same thing: burnout, impossible schedules, and zero support. The system was broken.
Instead of another band-aid solution, Sarah applied the 'Systems' pillar of RAMS.
Diagnostic Phase: She started with anonymous, facilitated listening sessions (not another useless survey) to get real, qualitative data. She quickly discovered the root issue wasn't pay; it was a chaotic scheduling system that completely ignored childcare needs and offered zero predictability, causing immense stress.
System Redesign: Sarah didn't impose a solution. She worked with a small team of nurses to co-design three new scheduling models that prioritized predictability and team-based assignments, which allowed for more consistent patient loads and stronger peer support.
Implementation & Feedback: She then piloted the most popular model on a single unit for 90 days. It wasn't perfect, but by creating a transparent feedback loop, her team felt heard and empowered to help refine it.
The result wasn't just a process change; it was a cultural one. By addressing the systemic root cause of the stress, Sarah showed her team that leadership was about creating an environment where they could thrive, not just survive. Within six months, turnover on that pilot unit dropped by half.
Case Study Two: Attitude and Mastery After a Critical Incident
Now, picture David, a clinical director whose department just went through a traumatic critical incident. The emotional fallout was immediate: fear, blame, and a palpable sense of dread hanging over the team. In the past, his default reaction would have been to focus only on the procedural review, completely ignoring the human toll.
This time, he consciously engaged the 'Attitude' and 'Mastery' pillars.
Attitude (Regulating the Room): David’s first priority was managing his own nervous system. He knew his calm, regulated presence was the only thing that could create psychological safety. He began the post-incident debrief not with blame, but with a simple acknowledgment: "This was incredibly hard, and I am here to support you all." That single statement shifted the energy from fear to solidarity.
Mastery (Embodied Skills): He then facilitated a structured debrief focused on learning, not fault-finding. He used his Mastery skills to hold space for the team's difficult emotions without becoming dysregulated himself. He drew a firm boundary against gossip and speculation, redirecting every conversation toward systemic vulnerabilities and what the team needed to feel supported.
By leading with a regulated Attitude and demonstrating emotional Mastery, David stopped the incident from fracturing his team. He turned a moment of potential collapse into a powerful opportunity for building resilience and trust.
This is the very essence of moving from a manager who just directs tasks to a leader who cultivates a thriving human system. For leaders looking to build these exact skills, the RAMS Accelerator provides the structured environment to develop this level of sovereign leadership.
Reclaiming Your Leadership Sovereignty
Let's be clear: the goal here isn't to single-handedly fix every systemic problem plaguing healthcare. That’s an impossible, exhausting task, a surefire recipe for accelerating burnout, not solving it.
The real path forward is mastering your own internal state so you can lead with unshakeable clarity amidst the chaos. This is the very essence of what I call leadership sovereignty.
Your regulated presence is your single most powerful asset. It’s the invisible force that calms a panicked room, inspires genuine trust in your team, and makes clear, decisive action possible when the stakes are highest. When your nervous system is grounded, your external impact is magnified exponentially.
Your Presence Is Your Power
This internal stability is not a "soft skill"; it's a strategic imperative. Every single decision you make, every interaction you have, is filtered through the state of your own nervous system. A dysregulated leader transmits anxiety, fueling confusion and reactivity across their team.
A sovereign leader, on the other hand, creates psychological safety. They build resilience and focus in their people not by force, but by their very presence.
This shift reframes leadership from an act of relentless doing to an act of intentional being. Your primary responsibility is not to have all the answers but to hold a steady center for those who look to you for guidance.
This is the return to yourself. It's about moving from a state of constant, soul-crushing depletion to one of sustainable, embodied power. Your energy, your focus, and your effectiveness are not commodities to be sacrificed on the altar of your career. They are the very foundation of your ability to lead.
The Next Step on Your Journey
Reclaiming this sovereignty is a deliberate process. It means unlearning the patterns that pushed you to the brink and installing new, sustainable systems for yourself, both personally and professionally. It all begins with a clear, honest assessment of where your energy is truly going and what deep-seated leadership patterns are holding you back.
This is your invitation to take that first, crucial step. It’s not about adding more to your already overflowing plate, but about fundamentally changing how you carry the load. By understanding your unique leadership archetype, you can begin the journey of reclaiming your focus, your energy, and your profound effectiveness.
Your Questions, Answered
When you're in the thick of it, navigating the labyrinth of healthcare leadership, it's easy to feel like you're facing these challenges alone. You're not. Here are some of the most common questions I hear from leaders trying to create real, lasting change, and my straight-to-the-point answers.
What Is the Single Most Impactful First Step to Address Team Burnout?
Stop trying to fix it. At least, not yet.
The most powerful first step you can take isn't launching another wellness initiative or a resiliency webinar. It's creating genuine psychological safety by shutting up and listening. I'm talking about structured, non-judgmental listening sessions where your only goal is to deeply understand your team's lived experience with the systemic friction that’s grinding them down.
This isn’t about brainstorming solutions on the spot. It's about gathering the raw, honest data you need to see the real problems, the chaotic scheduling, the soul-crushing administrative tasks, the chronic resource gaps. This act alone starts to build a foundation of trust. It also shifts your role from the overwhelmed "fixer" to a far more powerful and sustainable one: the "facilitator" of meaningful change, armed with the truth.
How Can I Justify Wellness Program Costs During Budget Cuts?
You have to change the conversation entirely. Stop framing it as an expense and start presenting it as a critical investment in cost avoidance and risk mitigation. This isn't fluffy stuff; this is hard-nosed business sense.
Get the data. Calculate the staggering cost of turnover for just one experienced nurse or physician in your organization, recruitment, onboarding, training, lost productivity. It's massive. Present your numbers clearly and position your leadership and wellness programs as what they are: essential retention tools that directly slash those replacement costs.
Better yet, a supported, regulated, and engaged team makes fewer mistakes. Fewer errors mean better patient safety scores and lower liability risk. This isn't a "soft" line item on the budget; it is a direct, measurable investment in your most valuable, and most expensive, asset: your people.
How Do I Apply RAMS When I Cannot Control Organizational Policy?
You start where you have 100% control: within your own sphere of influence. Forget about the policies you can't change for a moment and focus intensely on 'Attitude' and 'Mastery.'
You have complete authority over your own nervous system and how you show up for your team. By modeling calm, consistent, and clear-headed leadership, you create a powerful micro-culture of stability, a buffer against the organizational chaos raining down from above. That is your first move.
Next, you apply the 'Systems' principle to every single process your team touches. Streamline workflows. Clarify roles to kill ambiguity. Fiercely protect your team's time and energy from pointless distractions. By doing this, you create a pocket of excellence, a compelling case study with measurable results. Then, you can go to the higher-ups not with complaints, but with data-backed proof of what works, influencing wider policy from the ground up.
At Baz Porter, we specialize in guiding accomplished women leaders out of survival mode and into sovereign leadership. If you're ready to stop managing chaos and start architecting resilience, see how our methods can support your journey at https://bazporter.com.
